What is Hypertensive Nephropathy?
Hypertensive nephropathy refers to kidney damage resulting from prolonged high blood pressure (hypertension). Long-term hypertension strains the tiny vessels in the kidneys (glomeruli) and inhibits their ability to eliminate waste and water properly. Over time, this can lead to chronic kidney disease (CKD) or even kidney failure.
Causes & Risk Factors
- Chronic Hypertension – Long-term high blood pressure damages kidney blood vessels.
- Atherosclerosis – Cholesterol deposits harden arteries, reducing kidney blood flow.
- Diabetes & Obesity – Both conditions worsen hypertension-related kidney damage.
- Genetics – A family history of hypertension or kidney disease increases the risk.
- Age – Older adults are more susceptible due to prolonged exposure to high blood pressure.
- Excessive Salt Intake – Increases blood pressure, adding extra strain on the kidneys.
- Smoking & Alcohol – Contribute to hypertension and kidney stress.
Symptoms
Hypertensive nephropathy progresses gradually, often without noticeable symptoms until significant kidney damage has occurred. Common signs include:
Rising blood pressure (persistent and worsening)
Swelling in the face, ankles, and legs due to fluid retention
Frequent urination, especially at night (nocturia)
Fatigue and general weakness
Presence of protein in the urine (foamy urine)
Difficulty concentrating and poor memory
Nausea and loss of appetite
Diagnosis
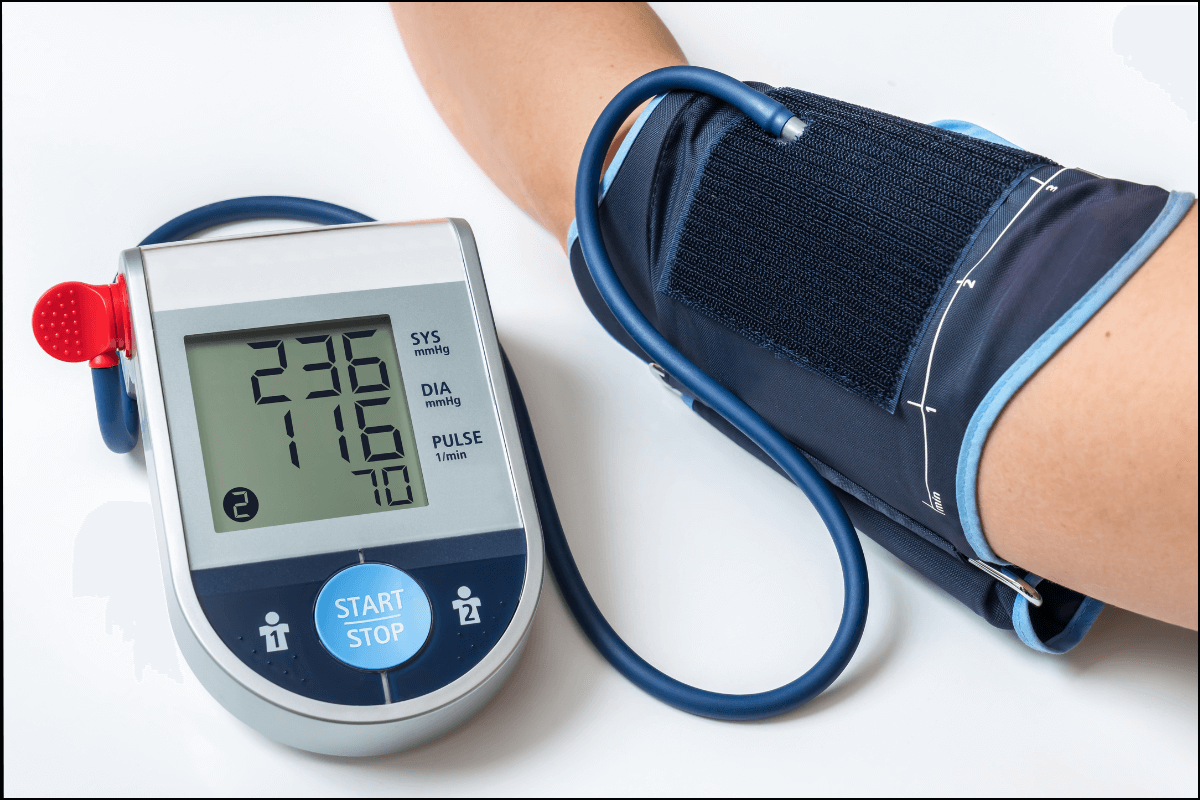
- Blood Pressure Monitoring – Consistently high readings indicate risk.
- Blood Tests – Check kidney function (Creatinine, BUN, GFR levels).
- Urine Tests – Detect protein (proteinuria) and other abnormalities.
- Ultrasound or CT Scan – Assess kidney size and structure.
- Biopsy (Rare Cases) – A tissue sample may be taken for detailed evaluation.
Treatment & Management
Since kidney damage from hypertensive nephropathy is often irreversible, treatment focuses on slowing disease progression and preventing kidney failure.
1. Blood Pressure Control
Target BP: Below 130/80 mmHg (recommended for kidney patients)
Medications:
- ACE Inhibitors (e.g., Lisinopril, Ramipril) – Protect kidneys by reducing pressure in the glomeruli.
- ARBs (e.g., Losartan, Valsartan) – Alternative for those intolerant to ACE inhibitors.
- Diuretics (e.g., Furosemide, Hydrochlorothiazide) – Help reduce fluid retention and lower BP.
- Beta-blockers & Calcium Channel Blockers – Used if additional BP control is needed.
2. Lifestyle Modifications
Low-Sodium Diet – Reducing salt intake helps lower BP.
Healthy Weight Management – Obesity worsens hypertension and kidney strain.
Regular Exercise – 30 minutes of moderate activity daily benefits BP and kidney health.
Avoid Smoking & Alcohol – Reduces kidney damage and strain.
Control Diabetes & Cholesterol – Poorly managed diabetes accelerates kidney deterioration.
Stay Hydrated – Supports kidney function and blood pressure regulation.
3. Routine Monitoring
Kidney Function Tests – Every 3-6 months to track kidney function.
Urine Tests – To monitor for protein leakage.
Blood Pressure Monitoring – Home tracking helps in adjusting treatment.
Complications
- Chronic Kidney Disease (CKD) → May progress to dialysis or kidney transplant.
- Heart Disease & Stroke → Hypertension affects multiple organs.
- Electrolyte Imbalance → Can lead to muscle weakness and heart problems.
Conclusion
Hypertensive nephropathy is a serious condition, but with proper management, it can be controlled. Early intervention through blood pressure control, lifestyle modifications, and regular monitoring can slow its progression and help prevent kidney failure.